Inside Infant-Parent Mental Health Care
 By Claudia M. Gold MD
By Claudia M. Gold MD
Inside Infant-Parent Mental Health Care
Three-month-old Jenna sleeps peacefully in her mother’s lap. The cards seem stacked against her. Cara at 17 is struggling to finish high school. She has been diagnosed in the past with bipolar disorder, but currently is receiving no treatment. Her primary care doctor, who referred her to me, has been prescribing an anti-anxiety medication as a temporizing measure. Cara has been playing phone tag for over a month with the therapist at the community mental health center, whom she needs to see in order to get an appointment with a psychiatrist.
Cara is scheduled as my patient in my behavioral pediatric practice. I put anxiety as the diagnosis on the billing form. But in truth the aim of my work with this mother-infant pair is to protect her daughter’s developing brain from the well-documented ill effects of maternal mental illness on child development.
Cara talks in a rambling manner about a range of subjects- her older sister at 20 pregnant with her second child, but neglectful of the first, her father who abandoned the family when she was two. She is particularly focused on her difficult relationship with James’ father, Ed. She tells of his drug use, his recent arrest for stealing, his neediness and his inability to accept his role as father.
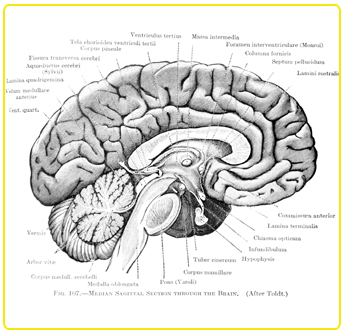
An infant’s brain makes as many as 1.8 million neural connections per second. The way in which these connections are formed is highly influenced by human relationships. As Cara responds to Jenna’ face and voice, is attuned with her rhythms and needs, both physical and emotional, she is literally growing her brain.
Important research has shown that when a mother can think about her baby’s mind and attribute meaning to his behavior, she helps him to develop a secure sense of himself and of his relationship with her. This security helps him to regulate himself in the face of difficult emotions. As he grows older he will have the capacity to think clearly and flexibly and manage himself in a complex social environment.
When I work with mother-baby pairs like Cara and Jenna, I focus on one simple thing. I listen to these mothers with the aim of helping them to reflect on their baby’s experience of the world and the meaning of their behavior. It never ceases to amaze me that with this singular focus, meaningful communication happens even in what appears to be chaotic and dismal circumstances.
As I listen to Cara’s rambling story, I know I need to help her start thinking about how all of this affects her relationship with Jenna. I use a technique I learned from leading researcher and clinician Peter Fonagy to help a person who is stuck in this kind of non-reflective thinking. I hold up my two hands. “Wait, I say. “I want you to help me understand how you think these problems with Ed connect with your relationship with Jenna.”
She pauses for a moment and then begins to cry. “When Jenna is so needy of me, it makes me think she’s just like her father, and I get so mad. Then I feel terrible for getting angry at her.” It’s a remarkable insight. But she isn’t done. She looks down at Jenna. “See how relaxed she is when I am calm. But when I get upset, she starts to cry.” Then she tells me of a time when she felt about to lose control, but somehow had managed to make Jenna laugh. “We were having a conversation,” she says joyfully, “even though she doesn’t say any words!”
It is a small moment in one 50-minute visit. I am confident, however, that with a string of moments like this, where Cara is fully present with her daughter, there is hope that she may break the cycle of intergenerational transmission of mental illness and help to grow a healthy brain.
About: Claudia M. Gold MD is a pediatrician with a longstanding interest in addressing children's mental health issues in a preventive model. She blogs at http://www.claudiamgoldmd.blogspot.com/




 1 Comment
1 Comment